
As a result, researchers must extract the information of interest from the graphical representation to use the data for their modeling approaches. Unfortunately, published data are typically presented in aggregate form as plots or graphs without providing access to the underlying raw, uncondensed data. However, for model development, time‐dependent data of pharmacological relevant processes are a crucial requirement. However, because the greatest pitfall comes from pre‐existing errors, we recommend always making published data available as raw values.ĭuring the past few years, quantitative systems pharmacology (QSP) and especially physiologically‐based pharmacokinetics modeling (PBPK) have proven to be an important cornerstone of model‐informed drug discovery and development. Our findings suggest that data digitizing is precise and important. Analysis of 181 literature peak plasma concentration values revealed a considerable discrepancy between reported and post hoc digitized data with 85% having ζ > 5%. Although significant, no relevant confounders were found (mean ζ ± SD circles = 0.69% ± 0.68% vs. Accuracy, precision, confounder influence, and variability were investigated using scaled median symmetric accuracy (ζ), thus finding excellent accuracy (mean ζ = 0.99%).
#Engauge digitizer online software#
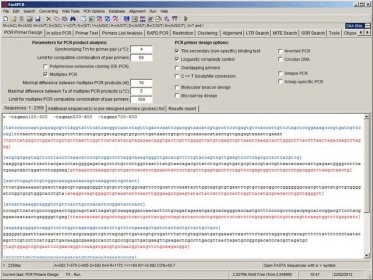
To quantify their relevance, a literature search revealed a remarkable mean increase of 16% per year in publications citing digitizing software together with QSP or PBPK. While investigators may be basing their effect sizes on prior data yet failing to cite sources in their protocols, clearly a need for better transparency exists.In quantitative systems pharmacology (QSP) and physiologically‐based pharmacokinetic (PBPK) modeling, data digitizing is a valuable tool to extract numerical information from published data presented as graphs. However, the primary end point ultimately determines the size, cost, and feasibility of a given trial.
#Engauge digitizer online trial#
For instance, a negative clinical trial can still provide valuable information regarding toxicity, convenience, and quality of life end points. The categorization of trials as either positive or negative is also somewhat simplistic, since these studies provide important information on secondary end points and allow subgroup analyses. Another caveat is that our study is a post hoc analysis, and as such we cannot distinguish a negative trial from an underpowered trial. Including these trials would increase the proportion of trials that did not demonstrate effectiveness of new interventions. Our analysis omitted trials that were closed early and were never published. However, this study has several limitations.
Of note, there are also important methodological differences between the evaluation of NCI sponsored trials in the two eras the current study only evaluated observed-to-expected HRs for time-to-event data, whereas the prior analysis included both HRs and odds ratios.

However, this did not increase the proportion of positive trials, which may illustrate the challenge of maintaining sustained progress in disease settings that have already experienced a substantial increase in survival over the past half century. bringing more promising therapies into phase III trials) may be responsible for this favorable finding. Improvements in clinical trial design and methodology as well as improved preclinical and early clinical screening (i.e. We found that this ratio appears to have decreased in modern NCTN clinical trials. Table 1 Characteristics of randomized controlled trials included in the analysisĪlthough it is unclear what the ideal ratio of observed-to-expected HRs should be, examining trends can inform us as to whether we are persistently overestimating effect sizes.


 0 kommentar(er)
0 kommentar(er)
